Introduction
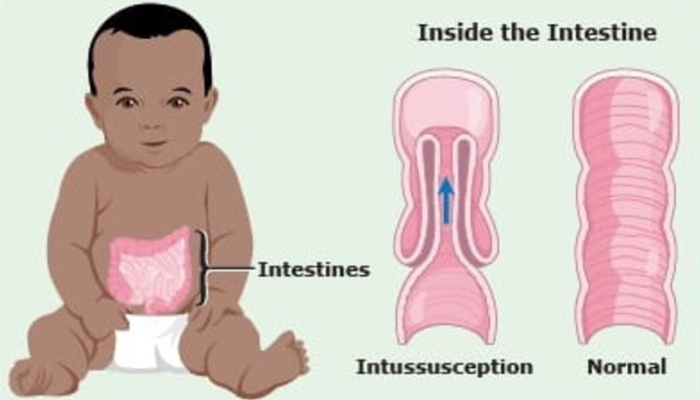
Intussusception is a common condition in childhood wherein one segment of the intestine telescopes into the other. It is most common in the first two years of life but it can affect all pediatric ages. It is a surgical emergency in children, and with timely intervention, the outcomes of treatment can be excellent.
Intussusception most commonly occurs as a consequence of a viral infection. In older children, a diverticulum of the intestine is often the instigating factor. Other lesions such as polyps or masses are the underlying cause in a minority of childhood cases. Such lesions are called pathological lead points. They are usually picked up during investigation for the intussusception and their presence or absence determines further therapy.
When one loop of bowel telescopes into the other, the bowel wall begins to swell, leading to blockage of the bowel lumen. Gradually, the blood vessels supplying the bowel wall get compressed. The bowel wall becomes weak in some areas making it susceptible to rupture. Complete occlusion of the blood supply can lead to bowel gangrene. Timely intervention is necessary to avoid these complications.
The most common symptom of Intussusception is crampy abdominal pain with or without vomiting. Between episodes of pain, the baby may appear surprisingly well. Many children have had symptoms of a viral infection or diarrhea in a preceding couple of days. During an episode of pain, the child typically draws his/her legs over the abdomen while crying. Another classic symptom is the passage of blood and mucus in stool, described as “red currant jelly stool”. Along with these symptoms, your doctor’s findings on examination of the child will lead to the suspicion of Intussusception. The diagnosis is confirmed by a radiological investigation, which is usually ultrasonography.
Treatment:
The therapy offered by your paediatric surgeon will depend on a number of clinical and anatomical factors. Generally, the surgeon would follow one of two approaches a) enema reduction and b) surgery.
1. Enema Reduction:
In recent years, this non-invasive therapy for Intussusception has become the first line of treatment in many cases. In this therapy, a paediatric surgeon uses radiological guidance to reduce the Intussusception ( which means to free the bowel) by instilling fluid rectally. The use of ultrasound to guide the procedure is popular because it is free of radiation risk.
In general, it is difficult to do the procedure after 48 hours of the onset of symptoms. Whether or not enema reduction can be attempted depends on the surgeon’s clinical judgement. Even in the best of hands, there remains a small but real risk of bowel perforation during enema reduction. Therefore, your surgeon will always have the child ready for surgery before attempting an enema reduction. This is because enema reduction can fail, or can be complicated by a rent in the intestine. In that case, the child needs to be operated on immediately, to minimise damage.
2. Surgery:
this was the classic treatment for Intussusception, before the advent of enema reduction techniques. Even today, a paediatric surgeon will decide to proceed straight to surgery, especially if the symptoms have been present for more than two days, the child’s bowel seems obstructed, the anatomy of the intussusception is not amenable to enema reduction, or the surgeon suspects that there may be a mass or lesion causing the intussusception and which needs to be removed.
The surgery may be limited to simple manual reduction of the intussusception or may require more extensive procedures such as the removal of a part of the bowel. If any bowel has been removed, it will be sent to a histopathologist for examination. This is to detect any underlying illness that will require more extensive therapy.
Intussusception can recur after therapy and the surgeon will continue to remain vigilant after an enema reduction or surgery. The risk of recurrence is 4-10% after enema reduction and 3-5% after surgery. That is to say that more than 90% of children will not have a repeat episode. There is nothing that can really be done to prevent an intussusception. Attention to food hygiene is all that can be recommended.