Hearing that your child needs any kind of surgery can be overwhelming. When the procedure involves their chest or lungs, the anxiety can be even greater. If your doctor has recommended a Video-Assisted Thoracoscopic Surgery (VATS), you likely have many questions. This guide is designed to help you understand what a VATS procedure is, why it might be needed for your child, and what to expect during recovery.
Understanding VATS: Minimally Invasive Chest Surgery
Video-Assisted Thoracoscopic Surgery (VATS) is a minimally invasive surgical technique used to diagnose and treat problems inside a child’s chest, such as in the lungs, pleura (the lining of the lungs), or the space around the lungs.
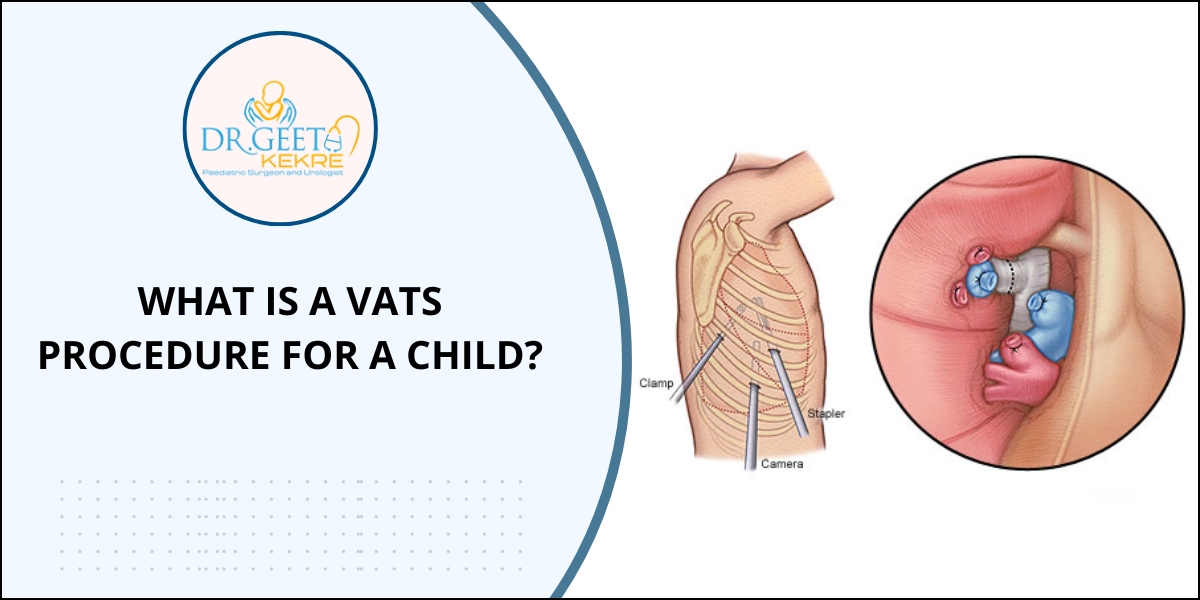
Unlike traditional “open” thoracic surgery that requires a large incision and spreading the ribs, VATS is performed using a tiny camera called a thoracoscope. The surgeon makes several small incisions (typically 3-4, each about 1-2 centimeters long) between the ribs. The thoracoscope transmits live video of the inside of the chest onto a monitor, allowing the surgeon to operate with specialized, long-handled instruments.
Why Might a Child Need a VATS Procedure?
Pediatric surgeons use VATS for a variety of conditions. Some of the most common reasons include:
- Lung Biopsy: To take a small sample of lung tissue for diagnosis.
- Treatment of a Spontaneous Pneumothorax: A collapsed lung that can occur in tall, thin adolescents, often repaired by blebectomy and pleurodesis.
- Empyema Drainage: To drain a collection of infected fluid from the pleural space around the lung.
- Lobectomy: Removal of a lobe of the lung, often for congenital lung malformations like Congenital Pulmonary Airway Malformation (CPAM) or sequestration.
- Biopsy of Masses or Lymph Nodes: To investigate tumors or infections.
The Key Benefits of VATS for Children
The minimally invasive nature of VATS offers significant advantages for pediatric patients compared to open surgery:
- Less Pain: Smaller incisions mean less damage to muscles and nerves, resulting in significantly less post-operative pain.
- Shorter Hospital Stay: Children who undergo VATS often go home in 1-3 days, compared to a week or more with open surgery.
- Quicker Recovery: With less pain and smaller wounds, children can return to normal activities, including school, much faster.
- Reduced Scarring: The procedure leaves several tiny scars instead of one large, prominent one.
- Better Cosmetic Outcome: The small incisions are much less noticeable as the child grows.
While VATS is a highly advanced technique, it requires a surgeon with specialized training in pediatric minimally invasive surgery. It’s important to discuss the surgeon’s experience and the potential risks, which can include infection, bleeding, or air leakage, though these are relatively uncommon.
Recovery After a Pediatric VATS Procedure
Recovery is typically swift. Your child will be encouraged to breathe deeply and move around as soon as possible to prevent complications. Pain is managed effectively with medication. Most children resume light activities within a week or two, though contact sports may be restricted for a few weeks to allow the small incisions to heal fully.
Knowing that VATS is a modern, gentle approach can provide immense comfort. It’s a procedure designed to resolve serious conditions while prioritizing your child’s comfort and rapid return to being a kid.
Frequently Asked Questions (FAQs)
1. How long does a VATS procedure take for a child?
The length varies depending on the complexity, but most VATS procedures for children take between 1 to 3 hours.
2. What is the success rate of VATS in children?
VATS is highly successful, with success rates often exceeding 90-95% for common procedures like treating pneumothorax or empyema, and low complication rates.
3. Is VATS painful for a child?
While there is post-operative pain, it is significantly less than with open chest surgery. Pain is managed effectively with medications, and most children describe it as manageable discomfort.
4. What is the difference between VATS and open lung surgery?
VATS uses several small “keyhole” incisions and a camera, while open surgery (thoracotomy) requires one large incision and spreading the ribs. VATS offers less pain, faster recovery, and smaller scars.
5. Can a child live a normal life after a lung lobectomy via VATS?
Yes. The human lungs have remarkable reserve capacity. A child who has a lobe removed can expect to live a completely normal, active life with no limitations once fully recovered.